
This topic has been on my mind increasingly over the last few months. Explant surgery doesn't seem to be getting easier - hell, I often feel that it's getting harder but that may be a consequence of me constantly altering my own expectations.
I think that over time, I am expecting more of my own outcomes, so rather than me doing exactly what I was doing 5 years ago, only faster, I'm doing a hell of a lot more than I was 5 years ago (to get better results) and sometimes it means I'm probably taking longer than I once did for the same operation. That can end up being a bit of trap, because the more complexity you add to a procedure, the more steps, the harder it is to know exactly which steps matter.
Anyway, that is just a preamble to discuss one of my patients groups who I think faces the greatest challenge after explant surgery, and that is slim women with very small natural breasts who have large breast implants. The reasons I made those opening comments about doing a lot more in my explant procedures is because that typifies how I approach ladies with a small breast. We really do need to work a lot harder for those ladies to ensure they get good results. A bigger breast on the other hand doesn't require as much "work" - the volume of tissue allows us to let the breast do its own thing with very acceptable outcomes. If we let a small breast just do its own thing...well, unfortunately that leads to problems.
I say quite a bit to patients that it is easier to make something out of something, than it is to make something out of nothing. That is kind of self-evident I guess, but in terms of explant surgery it bears repeating.
The more natural tissue we have to use, the easier it is to make the breast look like a breast after explant surgery. Couple of reasons for that. Obviously, with more tissue there is more "stuff" that we can reshape and mould into a breast form. Less obviously, with more natural tissue there is often less stretch having to be applied to the skin, because it is the breast tissue that carries the weight of the implant and which supports it over time, which means the skin may be more robust at the time of explant with greater retained elasticity. The least obvious aspect of this is that with more natural breast tissue, there is greater weight to the reformed breast after explant, and this has a direct consequence on the predictability of the infra-mammary crease position (and by inference, whether the scar sits exactly as we want it to).
But when we see a patient with very sparse tissue volume, and large implants, then we are often having to deal with the challenge of creating shape without volume, managing an unpredictable crease position over time, and reapplying tension to the skin (after is has already been stretched) .
So let's look at each of these points in turn.
Shape without volume:
I think there are two overlapping themes here: 1) we have to consider shape as it relates to the boundaries of the breast and 2) we have to consider the effect of thinning of the breast tissue, which is most apparent in small-breasted ladies with large implants.
The breast boundaries are such an important aspect of defining natural anatomy, and therefore they play a huge role in explant procedures. The discussion of breast boundaries leads into the issue of the infra-mammary crease, but that deserves it's own separate focus based on the question of predictability (see below).
The importance of the breast boundaries comes back to the destructive nature of breast augmentation. We can't hide from the fact that in MANY breast augmentation procedures, there is a deliberate destruction of natural anatomy to facilitate the placement of a breast implant. Whether that be the lower of the breast crease, the cutting of the Pectoralis major muscle, the separation of breast tissue from the front of the Pec muscle (which results in the muscle riding up and become fixed by scar in an unnatural high position), the weakening of the muscle fibres which insert onto the sternum (and sometimes the deliberate thinning out of the cleavage area to allow an implant to sit medially resulting in a very close cleavage), and of course, the widening of the breast by destroying the lateral breast boundary to allow a broad implant to be placed. All of these steps which are often routine in cosmetic breast augmentation have a bearing on the type of breast we are then confronted with at the time of explant. In my opinion, each of these destructive steps needs to be considered, assessed and individually repaired during explant if we want to reform a small breast that looks aesthetically pleasing.

The related issue of thinning of the breast tissue arises both due to the steps taken by the surgeon, but also due to the presence of a large implant in a small breast leading to compression of the breast tissue into a thinned-out "rind" around the implant over time. This consequence of breast augmentation is especially challenging in cases with prepectoral implants because we see that thinning right behind the nipple (this is less of a feature of subpectoral implants) which is what leads to the classic concave breast with nipple retraction that may be seen after prepectoral explants.
Thinning is a challenge to address. One option (the easy option in a way) is to use fat transfer to create thickness. But given that we are talking here about slim, small breasted women, that isn't always a great option. Another option is a mastopexy, which allows us to stack tissue elements on top of each other, creating a degree of thickness. Again, this may not be an option in small breasted women but in some cases it is essential as a means to addressing skin laxity - see below in the section on skin tension.
What we also have to accept is that creating shape for women with very small breasts may have postural variation, and we can definitely see issues like a lack of volume in the inner aspect of the breast which results in a hollowness there, especially when lying down. If there is enough fat to transfer a meaningful volume, that problem may be solvable. If there isn't...well, sometimes we do struggle to undo the damage of breast implants, and this is one area where that is a possibility.
So, we have to think about ways to manipulate the thinned breast tissue to create thickness without relying on those addition procedures. The way that I do that (when I'm not doing a "proper" mastopexy) is using what might be termed an "internal mastopexy" (yes, I just made that up; no, it isn't a "thing" that you'll find by googling ). Essentially, I have stumbled onto a technique in which rows of sutures are placed in the breast tissue from the inside which has the effect of pleating the breast tissue to create thickness. This has to be done very carefully to avoid creating distortion of the skin, but it's a very nice technique in these cases.

The unpredictable breast crease (and why that happens):
This is something that I think I have only really started to understand myself in the last few years. To be honest, surgeons have debated the breast crease for years in different contexts - the question of whether the breast crease changes (and how) in breast procedures (especially breast reductions and mastopexies), whether the crease needs to be surgically manipulated, and what the underlying anatomy is the leads to the crease forming (as well as its variability amongst women).
What is increasingly clear to me is that the small-breasted women with large implants whose crease has been lowered at the time of breast augmentation (to accommodate a large implant) are a uniquely challenging group, but I have some ideas about how we best manage them. One thing (which is endlessly repeated by other surgeons) that I TOTALLY disagree with is this idea that we should just "let the crease find its own level". That is a recipe for inevitable problems in my experience.
The major issue for small breasted ladies (as compared to those with a fuller natural bust) is that once their implants are removed, the weight of the breast pushing down onto the crease (wherever it sits) is dramatically reduced. So in a way, we can summarise the effect of explant on the crease with one word: "gravity".
A really interesting observation that I have made regarding ladies with a smaller bust is this: whilst a lady with bigger natural breasts will see a stable breast shape and position at around 4 months, for the small-breasted ladies, this process can easily take 12 months or more. I put this down to the fact that with less breast "weight" acting on the lower pole and the breast crease, it just takes longer for things to stabilise and it we are more reliant on the behaviour of scar tissues to determine the breast shape/position and the relationship of the breast crease to the inframammary scar.
So the small breasted ladies will see the natural breast crease (which arises in part based on where the natural tissue sits) rise after explant. Therefore, we have to anticipate that by also elevating the previously lowered or weakened breast crease to try to increase the chance that the scar sits perfectly in the crease.
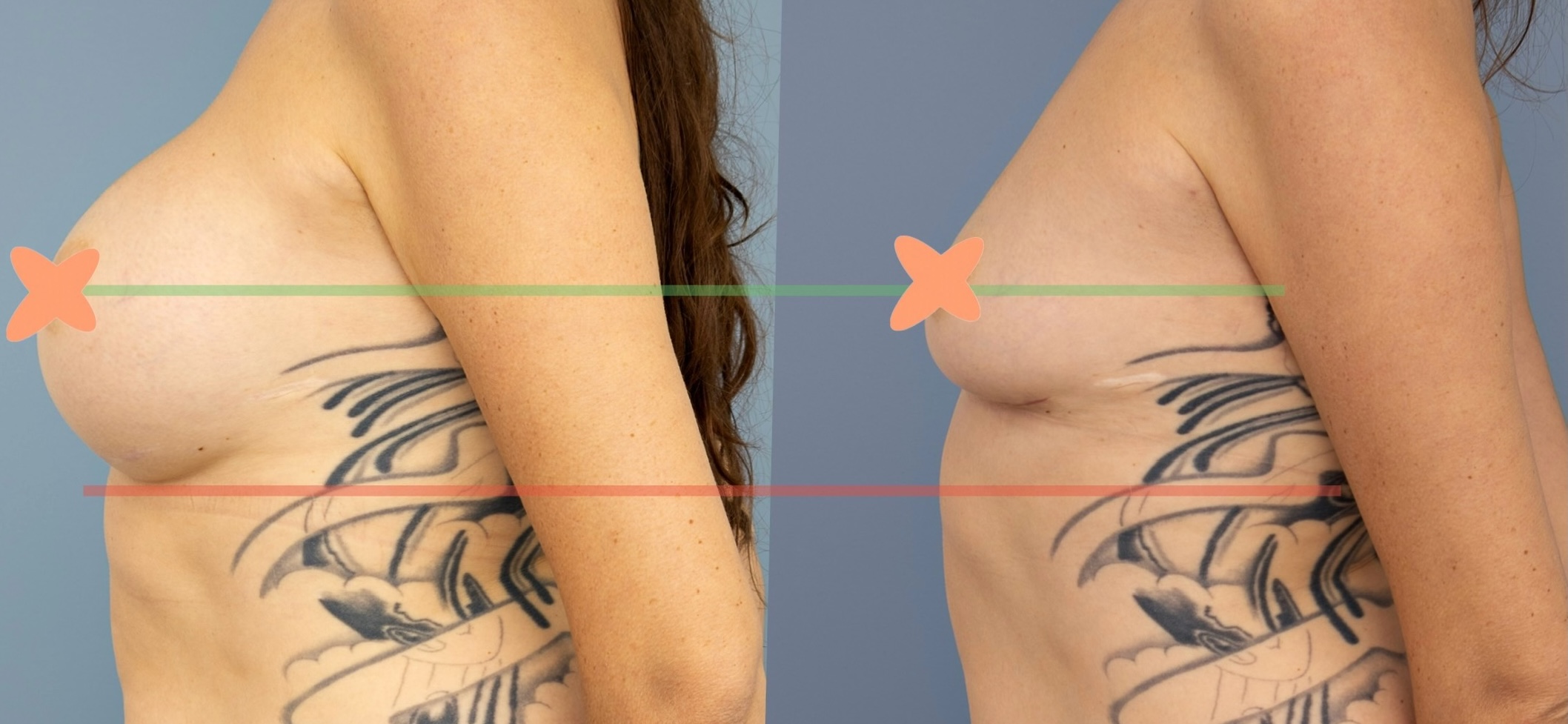
Now two things can go awry there: 1) the reconstructed inframammary scar will potentially subside a little over time resulting in the scar dropping away from/ out of the breast crease and 2) we might not have perfectly anticipated just how high the natural crease will sit.
So, as a consequence, the very small breasted ladies are a specific group with a higher risk of needing some sort of scar revision to reposition the scar back into the breast crease even when things look good at the start. Frustratingly I do have a couple of patients whose scars were well seated into the crease at 6 weeks and then by 4 months we see some separation of scar and crease - alas, I'm not perfect!
.jpeg)

Skin tension:
The final question of skin tension is the most variable of these issues because it has more to do with genetics and life events than it does with the surgery performed. As I mentioned above, in the absence of robust breast tissues, the forces applied by an implant are directly transmitted to the skin resulting in stretching, sometimes to the point that the natural elasticity of the skin is overwhelmed. This is different from person to person, and it is hugely influenced by other life-events like pregnancy.
Regardless though of whether the skin elasticity is preserved, the question that must be asked is at which point does a small breast lady with large implants that have stretched her breast require a mastopexy to address that stretch once the implants have been removed?
This is not an easy question, but the way it seems to work (for small breasted ladies) is this:
If you don’t have a mastopexy, even if you think you need one, and your breast "goes back to normal", then you didn’t need a mastopexy. If you need a mastopexy, this won’t happen.
If you need a mastopexy and you (or perhaps your surgeon) decide not to do that - perhaps you saw some surgeon on a podcast talking about ideas like an "implant holiday", letting the breast "recover" after implant removal and hoping that the skin will somehow tighten up again - then what you'll end up with is a distorted, misshapen breast that is scarred into a suboptimal shape and position.
I see quite a bit that there are surgeons who promote this idea of avoiding a mastopexy, and they'll use an example to "prove" their point, but invariably that example is a lady who never needed a mastopexy in the first place. These ladies typically would have gotten better results if the surgeon had properly shortened and managed the lower pole, but a mastopexy was not the answer. So it certainly feels quite disingenuous.
The decision to do or not to do a mastopexy is one of the biggest questions in explant surgery where a surgeon’s judgement is in play. If you actually need a mastopexy and you don’t do it, hoping for magic skin tightening fairies to come along to save you…well, you’ll still need that mastopexy, but it is harder down the track than it is at the time of explant.
Have I got it wrong in the past? Maybe, yeah. I think I've done a couple of mastopexies when I didn't really need to, and equally I have not done them when perhaps I should have. It can be a tough call. But that doesn't mean we should shy away from actually making the call.
So, in some ways the question of skin tension is the question of whether a small breasted lady needs a mastopexy just to address the skin stretch that comes from large implants. And I think that patients can be divided into 3 groups:
The summary.
The challenge of explant surgery never decreases in my opinion. As time goes by, I find myself demanding more and more of my own outcomes. I worry a bit about that because it has the effect that I am rarely entirely satisfied, even though my patients are (I think) pretty happy with their results.
Explant surgery in small breasted women demands different techniques compared to how I approach the surgery in women with a larger breast. Unfortunately, I also see a higher proportion of explant revision patients who have small breasts, which suggests that the way explant surgery is being done more broadly isn't taking that fact into account.
A larger natural breast can hide all manner of sins, if the explant procedure is done poorly. The small breast leaves nowhere for the surgeon to hide.
So, if you're thinking about explant procedures and you do have a small natural breast, please make your decisions very carefully.